Table of Contents
In early July 2023, a chilling reminder of history emerged in Colorado. Public health officials confirmed a human case of bubonic plague in Pueblo County. This sent a ripple of concern through the state, conjuring images of the Black Death’s devastation in medieval Europe. While the event may seem like something out of a historical fiction novel, it highlights the importance of awareness and preparedness for even ancient diseases.
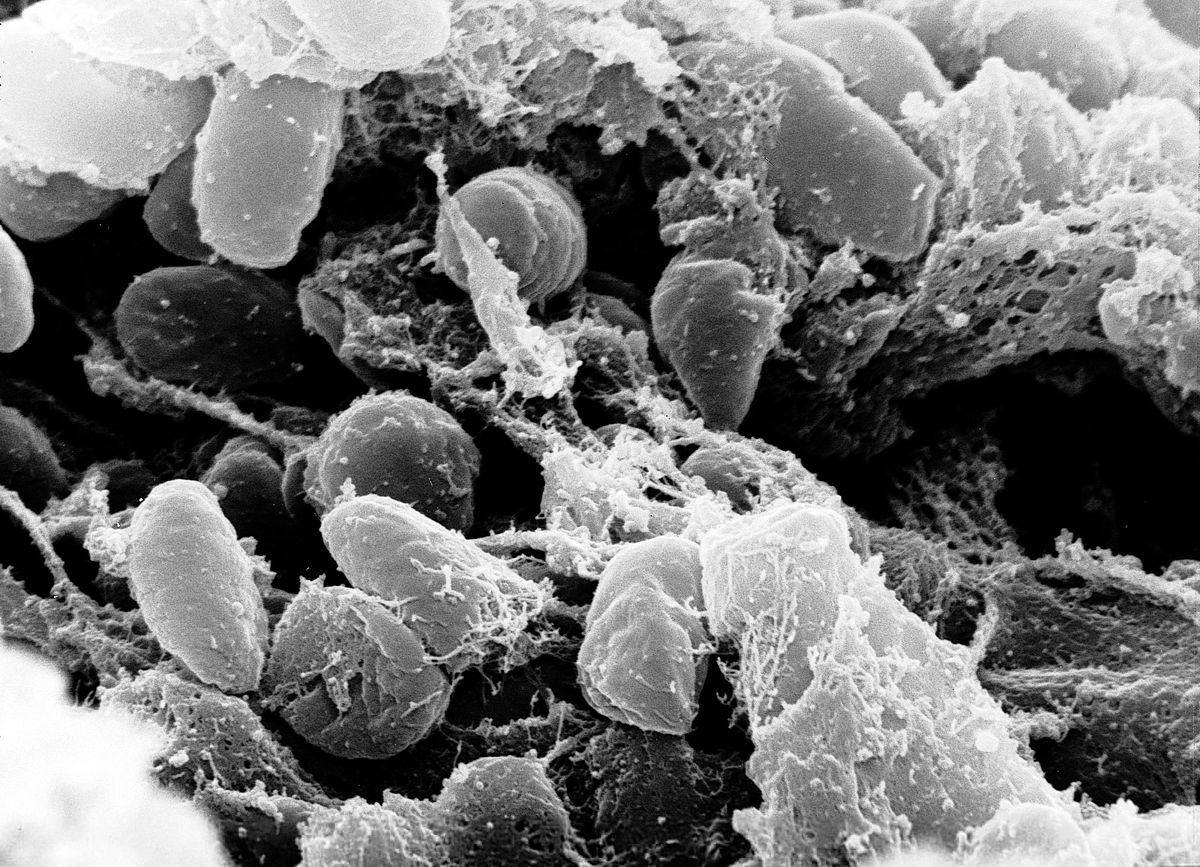
The Plague: A Bacterial Foe
Yersinia pestis, the bacterium responsible for the plague, is a fascinating and rather resilient foe. Let’s delve deeper into its characteristics and the different forms of plague it can cause.
Yersinia pestis: A Master of Deception
This gram-negative bacterium is a true survivor. It possesses a unique capsule that shields it from the human immune system. Additionally, Y. pestis can “hide out” within the cells of the lymphatic system, further hindering immune response. Here are some key aspects of this cunning pathogen:
- An Arsenal of Weapons: Y. pestis has a number of virulence factors, essentially molecular tools that help it establish infection. These include toxins that damage host cells and enzymes that help it avoid immune detection.
- A Feast for the Fleas: Yersinia pestis has a remarkable relationship with its flea vectors. The bacteria can form biofilms within the flea’s foregut, blocking it and causing the flea to vomit repeatedly. This “vomit” transmission is a highly effective way for the plague to spread between rodents.
- Adapting to Survive: Y. pestis has evolved alongside rodents for millennia, constantly adapting to ensure its survival. This adaptability makes the development of new treatment options and preventative measures an ongoing challenge.
The Many Faces of Plague: Beyond Bubonic
The bubonic plague, characterized by swollen lymph nodes (buboes), is the most well-known form. However, Y. pestis can cause other types of plague, each with its own distinct features:
- Septicemic Plague: This aggressive form occurs when the bacteria enter the bloodstream and multiply rapidly. Symptoms include high fever, chills, weakness, and possibly skin discoloration due to internal bleeding. Untreated, septicemic plague can be fatal.
- Pneumonic Plague: This highly contagious form involves the infection of the lungs. It spreads through the inhalation of infected droplets coughed up by a person or animal with pneumonic plague. Symptoms include difficulty breathing, cough (possibly with bloody sputum), and high fever. Early diagnosis and treatment are crucial for survival.

A Reminder of Our Constant Dance with Microbes
The plague serves as a powerful reminder of the dynamic relationship between humans and microbes. While advances in medicine have significantly reduced its lethality, the ongoing threat highlights the need for continued research and public health vigilance. Understanding Yersinia pestis, its transmission routes, and the different forms of plague empowers us to take preventive measures and respond effectively if necessary.
A Modern Case with an Ancient Past
The recent bubonic plague case in Colorado wasn’t just a medical curiosity; it was a chilling echo of a disease that has haunted humanity for millennia. While the Black Death of the 14th century remains the most infamous outbreak, the plague’s history stretches back much further, leaving a trail of devastation across continents and cultures.
From Antiquity to the Black Death:
- Early Traces: Evidence suggests the plague may have been present as early as 3000 BC, with potential references in ancient Mesopotamian texts. However, definitive identification through bacterial analysis is challenging for such distant eras.
- The Plague of Justinian (541-542 AD): This devastating pandemic, named after the Byzantine emperor Justinian I, is considered the first major plague outbreak in recorded history. It ravaged the Eastern Roman Empire and beyond, causing widespread death and economic disruption.
- The Black Death (1346-1353 AD): This horrific event, believed to be a resurgence of the plague, decimated Europe. Estimates suggest it killed between 30-50% of the population in some regions, leaving a lasting social, economic, and psychological scar.

The Plague After the Black Death:
The plague didn’t vanish after the Black Death. It continued to erupt in Europe and other parts of the world for centuries, often following trade routes and causing localized outbreaks. The Great Plague of London (1665) is a chilling example, killing an estimated 100,000 people in a single year.
Beyond Europe: A Global Scourge
The plague wasn’t confined to Europe. Historical records and archeological evidence suggest outbreaks occurred in Asia, Africa, and the Middle East. The arrival of Europeans in the Americas tragically introduced the plague to the New World as well, contributing to the decimation of indigenous populations.
The Rise of Modern Medicine and a Changing Landscape
The discovery of antibiotics in the 20th century revolutionized the treatment of the plague. Early diagnosis and appropriate antibiotic therapy significantly reduced the mortality rate. Additionally, improved sanitation and hygiene measures helped control the spread of the disease by targeting flea populations, the primary vectors.
A Modern Resurgence? The Colorado Case in Context
While the Colorado case may seem like a historical anomaly, it’s not entirely unexpected. The plague persists in wild rodent populations around the world, including ground squirrels in the western United States.
The key takeaway from the Colorado case isn’t to panic, but to be aware. Modern medicine can effectively combat the plague, but vigilance and preventative measures remain crucial.
By understanding the plague’s long and complex history, we gain valuable insights into its potential for future outbreaks. This knowledge empowers us to prepare and respond effectively, ensuring that this ancient disease doesn’t cast a long shadow on our future.
The Pueblo Case: Unraveling the Mystery
The recent bubonic plague case in Pueblo County, Colorado, presented a puzzle for public health officials. Unlike historical outbreaks where the source of infection was often readily apparent, this case demanded a more nuanced investigation, akin to a detective story in the realm of public health.
Following the Trail of Yersinia Pestis:
- Patient Zero: The first step involved gathering information about the infected individual. Did they have any recent contact with areas known for plague activity? Were they involved in outdoor activities that could have exposed them to rodents or fleas? Maintaining patient privacy is paramount, but details that don’t reveal identity can be crucial for piecing together the puzzle.
- Environmental Investigation: Public health teams likely scoured the patient’s residence and surrounding areas for signs of rodent activity. This might involve setting traps to capture rodents for testing, as well as inspecting for potential flea harborages like burrows, tall grass, and areas with debris.
- Contact Tracing: Anyone who had close contact with the infected individual would be identified and monitored. This could include family members, co-workers, or anyone who may have shared a space where flea transmission was a possibility.
- Veterinary Involvement: Did the patient have any pets, particularly cats or dogs? These animals can come into contact with infected fleas and potentially become carriers themselves. Veterinarians would likely be involved in examining pets and recommending appropriate flea and tick control measures.
Beyond the Individual: Protecting the Community
The Pueblo case wasn’t just about the infected individual. Public health officials also implemented broader measures to safeguard the community:
- Public Awareness Campaigns: Educational materials would be disseminated to inform residents about the plague, its symptoms, and preventative measures.
- Increased Rodent Control Efforts: Areas with high rodent activity might see intensified trapping and baiting programs to control rodent populations and reduce the risk of flea transmission.
- Collaboration with Local Agencies: Public health officials likely collaborated with agencies like animal control and vector control to ensure a coordinated response.
The Importance of a Prompt Response
By swiftly initiating these investigative and preventative measures, public health officials aimed to:
- Limit Further Transmission: Identifying the source of infection and potential exposures helps prevent the spread of the plague to others.
- Provide Early Treatment: Early diagnosis and antibiotic therapy are crucial for a successful recovery from the plague.
- Reduce Public Anxiety: A transparent and informative public health response can alleviate community fear and promote appropriate precautions.
A Call for Vigilance, Not Panic
The recent bubonic plague case in Colorado understandably raises concerns. However, it’s crucial to maintain a balanced perspective. Here’s why panic isn’t the answer, and what we can do to ensure vigilance:
Modern Medicine vs. Medieval Mayhem:
The Black Death, the most infamous plague outbreak, ravaged Europe in the 14th century with a mortality rate exceeding 50% in some regions. This devastation stemmed from a lack of understanding about the disease, limited treatment options, and poor sanitation practices. Thankfully, the landscape has drastically changed.
- Antibiotics: The discovery of antibiotics in the 20th century revolutionized plague treatment. When diagnosed and treated promptly with antibiotics, bubonic plague has a very high survival rate (over 95%).
- Improved Diagnostics: Modern diagnostic tools allow for rapid and accurate identification of the plague bacterium, enabling swift treatment initiation.
- Public Health Infrastructure: Developed countries have robust public health systems with the capacity to investigate outbreaks, implement control measures, and educate communities.
Living with Rodent-Borne Diseases:
The plague bacillus (Yersinia pestis) persists naturally in rodent populations in certain parts of the world, including the western United States. This doesn’t mean an automatic outbreak is imminent. Public health officials constantly monitor rodent populations for signs of plague activity. Additionally, proactive measures like flea control on pets and rodent control programs in high-risk areas help minimize the risk of transmission.
Knowledge is Power: Taking Preventative Measures
While the risk of plague for the general public remains low, vigilance is key. Here are some simple steps you can take:
- Be Mindful of Rodent Activity: Seal up cracks and holes in your home’s exterior to prevent rodent entry. Keep your yard free of debris and eliminate potential nesting sites.
- Minimize Contact with Wild Animals: Avoid handling sick or dead rodents. If you must remove a dead rodent, wear gloves and dispose of it properly.
- Protect Your Pets: Talk to your veterinarian about flea and tick prevention for your pets, as they can come into contact with infected fleas.
- Stay Informed: Public health departments are your trusted source for accurate information. Stay updated on any advisories or recommendations specific to your area.
By working together and taking these simple precautions, we can ensure the plague remains a historical footnote, not a public health threat. Remember, knowledge and preventative measures are our best weapons against this ancient disease.
Focus on Preparedness, Not Panic
The Pueblo case serves as a reminder to be prepared, not panicked. Public health officials are well-equipped to handle such situations. By staying informed and taking preventative steps, we can minimize the risk of plague transmission and ensure the safety of our communities. Let’s focus on proactive measures and a collaborative approach to keep the plague in its rightful place – the past.
Looking Forward: Research and Preparedness
The recent Colorado plague case underscores the importance of continuous research and preparedness efforts. While modern medicine offers effective tools to combat the plague, complacency can be dangerous. Here’s why ongoing research and a proactive approach are crucial for the future:
The Evolving Threat: Antibiotic Resistance
The specter of antibiotic resistance looms large. Overuse and misuse of antibiotics can create strains of bacteria resistant to these life-saving drugs. While current antibiotics are still effective against the plague, research into alternative treatment options is essential. This could involve developing new antibiotics or exploring the potential of other therapies like phage therapy (using viruses to target bacteria).
Beyond Antibiotics: A Multi-Pronged Approach
Research efforts extend beyond just antibiotics. Here are some promising avenues for future advancements:
- Improved Diagnostics: Faster and more accurate diagnostic tests can expedite treatment initiation, improving patient outcomes and helping to contain outbreaks.
- Vaccines: While no commercially available human plague vaccine exists currently, research on developing a safe and effective vaccine is ongoing. Such a vaccine could offer long-term population protection.
- Enhanced Surveillance: Continuously monitoring rodent populations for signs of plague activity allows for early detection and intervention before outbreaks occur. This may involve innovative technologies like environmental DNA (eDNA) sampling to detect the presence of Yersinia pestis in the environment.
Building a Culture of Preparedness
Research is crucial, but it’s only one piece of the puzzle. Here’s how we can foster a culture of preparedness:
- Public Education: Ongoing public education campaigns can raise awareness about the plague, its symptoms, and preventative measures. This empowers individuals to take responsibility for their own health and protect their communities.
- Investment in Public Health Infrastructure: Strong public health systems with well-trained personnel, adequate resources, and robust communication networks are essential for effective outbreak response.
- International Collaboration: The plague doesn’t respect borders. Collaboration between countries on research, surveillance, and outbreak response strategies is vital to effectively manage the threat.
A Shared Responsibility: Protecting Our Future
The Colorado case serves as a wake-up call. It reminds us that even ancient diseases can pose challenges in the modern world. By investing in research, promoting preparedness, and fostering international collaboration, we can build a strong bulwark against the plague and ensure a safer future for generations to come. Ultimately, protecting ourselves from the plague is a shared responsibility – a responsibility we can best meet through knowledge, preparedness, and a commitment to public health.
Further Reading
